Gut Health: The Microbiome and Mental Health Connection

Discover the profound connection between your gut health and mental well-being. Learn more about the microbiome and its significant role in mental health. Take the first step towards a healthier, happier you. Visit Vibrant Vitality now.
Exploring the Link between Gut Microbiome and Mental Health
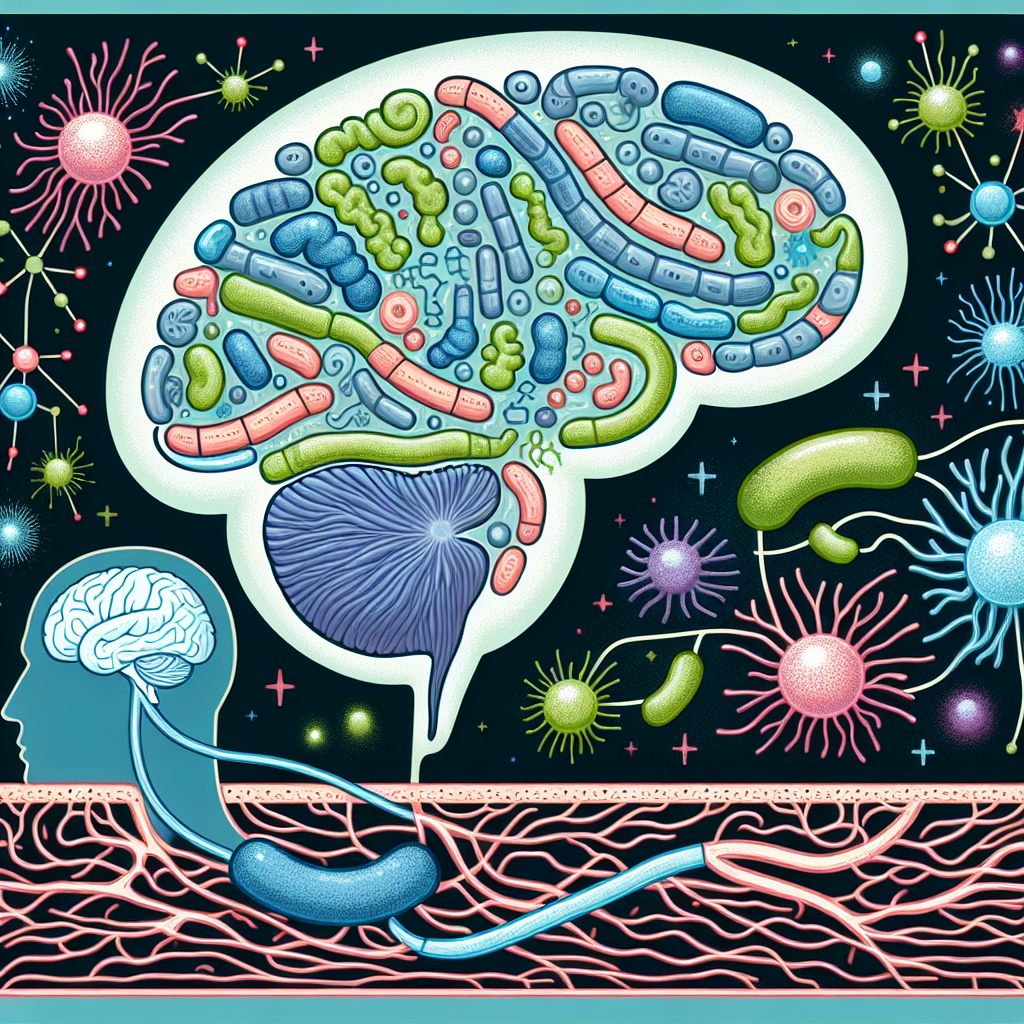
The human body is a complex ecosystem, home to trillions of microorganisms that play a crucial role in our overall health. Among these, the gut microbiome, a community of bacteria residing in our digestive tract, has recently been the focus of extensive research. Scientists are increasingly recognizing the profound influence of these gut microbes on various aspects of our health, including our mental well-being. This burgeoning field of study is revealing a fascinating link between gut health and mental health, suggesting that our diet and lifestyle choices can significantly impact our psychological state.
The gut microbiome is a dynamic entity, constantly interacting with our body and influencing our health in ways we are only beginning to understand. It aids in digestion, bolsters our immune system, and even produces essential vitamins. However, its role extends beyond physical health. Emerging research suggests that the gut microbiome can also affect our mental health, potentially influencing our mood, stress levels, and susceptibility to mental disorders.
This connection between the gut and the brain is facilitated by the gut-brain axis, a bidirectional communication pathway linking the central nervous system with the enteric nervous system. The gut and the brain communicate through various mechanisms, including neural, hormonal, and immune pathways. The gut microbiome can influence this communication, sending signals to the brain via the vagus nerve, a key component of the gut-brain axis.
One way the gut microbiome may impact mental health is through the production of neurotransmitters, chemical messengers that transmit signals between nerve cells. For instance, gut bacteria produce about 90% of the body’s serotonin, a neurotransmitter that regulates mood, sleep, and appetite. Imbalances in serotonin levels have been linked to depression and anxiety. Therefore, a healthy gut microbiome, producing adequate serotonin, could potentially contribute to mental well-being.
Moreover, the gut microbiome can influence the body’s stress response. Research has shown that gut bacteria can affect the hypothalamic-pituitary-adrenal (HPA) axis, the body’s central stress response system. Dysregulation of the HPA axis has been associated with mental health disorders such as depression and post-traumatic stress disorder. By modulating the HPA axis, the gut microbiome may help regulate our stress response and potentially mitigate the risk of these disorders.
Furthermore, studies have found correlations between alterations in the gut microbiome and mental health disorders. For example, individuals with depression or anxiety often exhibit differences in their gut microbiota compared to healthy individuals. While these findings do not establish causation, they suggest a potential role of the gut microbiome in these disorders.
However, it’s important to note that the research on the gut-brain axis is still in its early stages. While the evidence suggests a connection between the gut microbiome and mental health, many questions remain. For instance, it’s unclear whether changes in the gut microbiome cause mental health issues, or whether these issues lead to changes in the gut microbiome. Further research is needed to fully understand this complex relationship and its implications for mental health treatment.
In conclusion, the gut microbiome represents a promising frontier in mental health research. The emerging evidence of a gut-brain connection underscores the importance of maintaining a healthy gut microbiome, potentially through diet and lifestyle choices. As we continue to unravel the mysteries of the gut-brain axis, we may discover new ways to promote mental well-being and treat mental health disorders.
Understanding the Role of Gut Health in Anxiety and Depression
Gut health, a topic that has been gaining significant attention in the medical and wellness communities, is now being linked to mental health. The human gut, often referred to as the “second brain,” is home to trillions of bacteria, viruses, and fungi collectively known as the microbiome. This complex ecosystem plays a crucial role in our overall health, influencing everything from digestion to immunity. However, recent research suggests that the gut microbiome may also have a profound impact on our mental health, particularly in relation to anxiety and depression.
The gut and the brain are connected through a bidirectional communication system known as the gut-brain axis. This system allows the gut and the brain to send and receive signals to each other, influencing a variety of bodily functions. The gut microbiome plays a significant role in this communication system, producing various neurotransmitters and other chemicals that can affect our mood and mental health.
One of the key neurotransmitters produced in the gut is serotonin, often referred to as the “feel-good” hormone. Serotonin is involved in regulating mood, sleep, appetite, and cognitive functions. Interestingly, about 90% of the body’s serotonin is produced in the gut, highlighting the potential influence of the gut microbiome on our mental health.
Research has shown that individuals with anxiety and depression often have different gut microbiome compositions compared to those without these conditions. For instance, certain beneficial bacteria that produce serotonin and other mood-regulating chemicals may be less abundant in individuals with anxiety and depression. This suggests that an imbalance in the gut microbiome, known as dysbiosis, could potentially contribute to these mental health conditions.
Moreover, studies have found that probiotics, which are beneficial bacteria that can help restore a healthy gut microbiome, may have potential as a treatment for anxiety and depression. In several clinical trials, individuals who took probiotics reported improvements in their mood and anxiety levels. While more research is needed to fully understand the potential of probiotics in treating mental health conditions, these findings suggest that improving gut health could be a promising approach.
However, it’s important to note that the relationship between the gut microbiome and mental health is complex and likely influenced by many factors. For instance, diet, stress, sleep, and other lifestyle factors can all affect the gut microbiome and, in turn, mental health. Therefore, maintaining a healthy gut microbiome is likely just one piece of the puzzle when it comes to managing anxiety and depression.
In conclusion, the emerging research on the gut-brain axis and the role of the gut microbiome in mental health is truly fascinating. It suggests that our mental health may be more closely tied to our physical health than we previously thought. While more research is needed to fully understand this connection and how to harness it for therapeutic purposes, it’s clear that taking care of our gut health could have far-reaching benefits for our mental well-being. So, whether it’s through a balanced diet, regular exercise, stress management, or potentially probiotics, nurturing our gut health could be a key component in promoting mental health.
The Impact of Gut Microbiome on Brain Function and Mental Well-being
The human body is a complex ecosystem, home to trillions of microorganisms that play a crucial role in our overall health. Among these, the gut microbiome, a community of bacteria residing in our digestive tract, has been the subject of extensive research in recent years. Scientists are increasingly recognizing the profound impact of these microscopic inhabitants on various aspects of our health, including brain function and mental well-being.
The gut microbiome is not just involved in digestion, but also in the production of essential nutrients and the regulation of our immune system. Interestingly, it also communicates with the brain through what is known as the gut-brain axis. This bidirectional communication pathway allows the gut microbiome to influence brain function and behavior, thereby playing a significant role in our mental health.
The gut-brain axis operates through various mechanisms, including neural, hormonal, and immune pathways. The gut microbiome can produce neurotransmitters, such as serotonin and dopamine, which are critical for mood regulation. In fact, it is estimated that about 90% of the body’s serotonin, often referred to as the ‘happiness hormone’, is produced in the gut. This highlights the potential of the gut microbiome to influence our emotional state and mental health.
Moreover, research has shown that alterations in the gut microbiome composition can lead to changes in brain chemistry and function, potentially contributing to mental health disorders. For instance, studies have found associations between gut microbiome dysbiosis (imbalance) and various mental health conditions, including depression, anxiety, and autism spectrum disorder. While these findings do not establish causation, they suggest a potential role of the gut microbiome in the development and progression of these conditions.
The gut microbiome can also influence mental health through its role in the immune system. It helps regulate immune responses, and dysregulation can lead to chronic inflammation, which has been linked to mental health disorders. For example, research has shown that individuals with depression often have higher levels of inflammation. This suggests that the gut microbiome, through its influence on the immune system, could contribute to the development of depression.
The potential impact of the gut microbiome on mental health has opened up new avenues for treatment strategies. Probiotics, which are beneficial bacteria, and prebiotics, which promote the growth of beneficial bacteria, are being explored for their potential to modulate the gut microbiome and improve mental health. Early research suggests that these interventions could have positive effects on mood and anxiety symptoms, although more research is needed to confirm these findings and understand the underlying mechanisms.
In conclusion, the gut microbiome is emerging as a key player in brain function and mental health. The intricate communication between the gut and the brain, mediated by the gut microbiome, underscores the importance of maintaining a healthy gut for mental well-being. While much remains to be understood about this complex relationship, the current evidence points to the potential of harnessing the gut microbiome for mental health interventions. As research in this field continues to evolve, it is hoped that it will lead to novel strategies for the prevention and treatment of mental health disorders.