Understanding the Mind-Gut Axis in IBS and Anxiety

Discover more about the intriguing connection between your mind and gut, especially in relation to IBS and Anxiety. Uncover the secrets of the Mind-Gut Axis and how it can impact your overall health. Visit www.myvibrantvitality.com now.
Exploring the Connection between the Mind-Gut Axis and IBS
The human body is a complex system of interconnected parts, each playing a crucial role in maintaining overall health and well-being. One such connection, the mind-gut axis, has been the subject of increasing scientific interest in recent years. This bi-directional communication pathway between the brain and the gut has been found to play a significant role in various health conditions, including Irritable Bowel Syndrome (IBS) and anxiety.
IBS is a common gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits. It is a chronic condition that can significantly impact a person’s quality of life. Anxiety, on the other hand, is a mental health disorder characterized by excessive worry and fear. Interestingly, research has shown that these two seemingly unrelated conditions often coexist, suggesting a shared underlying mechanism. This is where the mind-gut axis comes into play.
The mind-gut axis refers to the communication network that links the central nervous system, which includes the brain, with the enteric nervous system, the network of nerves controlling the gastrointestinal tract. This connection allows the brain to influence gut function and vice versa. For instance, stress or anxiety can lead to changes in gut motility, secretion, and sensitivity, which can manifest as IBS symptoms. Conversely, gut disturbances can send signals to the brain, potentially triggering anxiety or exacerbating its symptoms.
The role of the gut microbiota, the trillions of microorganisms residing in our gut, is also crucial in this context. These microbes not only aid in digestion but also produce various substances, including neurotransmitters and metabolites, that can influence brain function. Dysbiosis, or an imbalance in the gut microbiota, has been linked to both IBS and anxiety.
Research has shown that individuals with IBS often have altered gut microbiota compared to healthy individuals. This dysbiosis can lead to increased gut permeability, commonly known as “leaky gut,” allowing harmful substances to enter the bloodstream and trigger an immune response. This can result in inflammation, which has been associated with both IBS and anxiety.
Moreover, certain gut microbes can produce neurotransmitters, such as serotonin and gamma-aminobutyric acid (GABA), which play a key role in regulating mood and anxiety. An imbalance in these microbes can therefore affect the production of these neurotransmitters, potentially contributing to anxiety.
The mind-gut axis also involves the hypothalamic-pituitary-adrenal (HPA) axis, the body’s primary stress response system. Chronic stress or anxiety can overactivate the HPA axis, leading to increased cortisol production. This can affect gut function and microbiota, further exacerbating IBS symptoms and potentially contributing to anxiety.
In conclusion, the mind-gut axis provides a fascinating insight into the complex interplay between the brain, gut, and microbiota. It offers a potential explanation for the coexistence of IBS and anxiety and opens up new avenues for treatment. For instance, interventions targeting the gut microbiota, such as probiotics, prebiotics, and dietary modifications, could potentially alleviate both IBS and anxiety symptoms. However, more research is needed to fully understand this complex relationship and to develop effective therapeutic strategies.
The Role of the Mind-Gut Axis in Anxiety and IBS
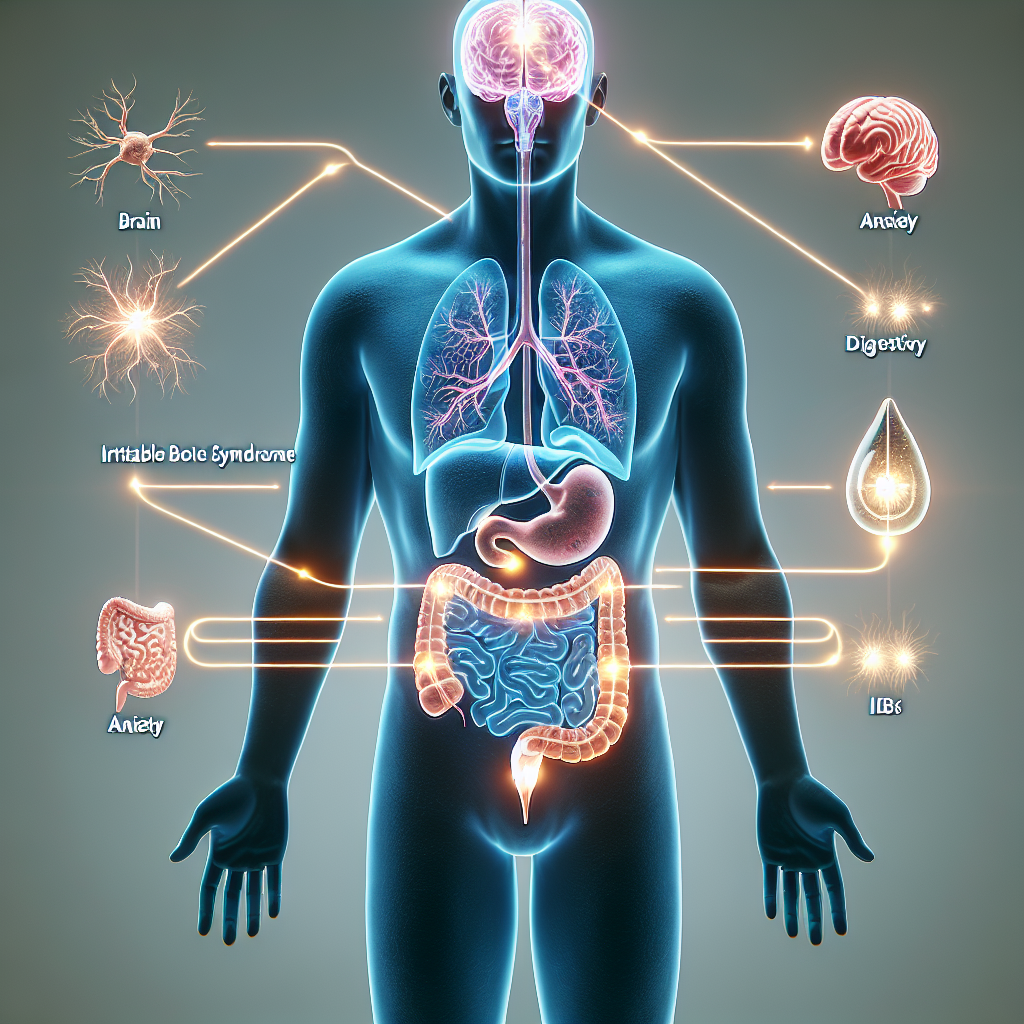
The mind-gut axis, a complex bidirectional communication system that exists between the central nervous system and the gastrointestinal tract, has been gaining increasing attention in the scientific community. This system plays a crucial role in maintaining homeostasis and is believed to be a contributing factor in various physical and mental health conditions, including Irritable Bowel Syndrome (IBS) and anxiety.
IBS, a common gastrointestinal disorder characterized by abdominal pain and altered bowel habits, is often associated with psychological distress. Anxiety, a mental health disorder characterized by feelings of worry, fear, or unease, is also frequently linked with gastrointestinal symptoms. The connection between these two conditions is not coincidental but is instead a manifestation of the mind-gut axis at work.
The mind-gut axis functions through a network of neurochemicals and hormones, allowing the brain and gut to communicate. For instance, the gut can signal to the brain when it’s full, and the brain can signal to the gut when it’s time to initiate digestion. However, when this communication system is disrupted, it can lead to a host of problems, including IBS and anxiety.
Research has shown that individuals with IBS often have an overactive stress response, which can exacerbate their gastrointestinal symptoms. This overactivity is thought to be due to a disruption in the mind-gut axis, where the brain’s stress signals are being sent to the gut, causing it to react. Similarly, individuals with anxiety often report experiencing gastrointestinal symptoms, such as stomachaches or diarrhea. This is because the brain’s anxiety signals can also be sent to the gut, causing it to react.
Furthermore, the gut itself is home to trillions of bacteria, collectively known as the gut microbiota. These bacteria not only aid in digestion but also produce various neurochemicals that can influence our mood and behavior. For instance, certain species of gut bacteria are known to produce serotonin, a neurotransmitter that regulates mood, sleep, and appetite. An imbalance in the gut microbiota, known as dysbiosis, can therefore disrupt the production of these neurochemicals, potentially leading to conditions like IBS and anxiety.
Interestingly, studies have shown that modifying the gut microbiota, such as through the use of probiotics or dietary changes, can help alleviate the symptoms of both IBS and anxiety. This suggests that the gut microbiota is a key player in the mind-gut axis and that targeting it could be a promising strategy for managing these conditions.
In conclusion, the mind-gut axis is a complex communication system that plays a crucial role in our physical and mental health. Disruptions in this system, whether due to stress, dysbiosis, or other factors, can lead to conditions like IBS and anxiety. However, by understanding the workings of the mind-gut axis, we can develop more effective strategies for managing these conditions and improving overall health. As research in this field continues to evolve, it is hoped that we will gain a deeper understanding of the intricate relationship between the mind and the gut, paving the way for novel therapeutic approaches.
Decoding the Complex Relationship between IBS, Anxiety, and the Mind-Gut Axis
Understanding the mind-gut axis in Irritable Bowel Syndrome (IBS) and anxiety involves decoding the complex relationship between these conditions. This relationship is a fascinating area of research that has gained significant attention in recent years. The mind-gut axis, a bidirectional communication system between the central nervous system and the gastrointestinal tract, plays a crucial role in maintaining homeostasis and influencing our overall health.
IBS, a common gastrointestinal disorder, is characterized by abdominal pain, bloating, and altered bowel habits. It is a chronic condition that significantly impacts the quality of life of those affected. Interestingly, a high percentage of individuals with IBS also suffer from anxiety and other psychological disorders. This observation led researchers to investigate the potential link between the gut and the brain, culminating in the concept of the mind-gut axis.
The mind-gut axis is a complex system involving hormonal, immunological, and neural pathways. It allows the brain to influence gut functions such as motility, secretion, and immune function, and vice versa. This bidirectional communication is crucial for maintaining gut health and responding to stress. However, when this communication is disrupted, it can lead to various health issues, including IBS and anxiety.
Research has shown that stress and anxiety can exacerbate IBS symptoms. This is because stress can alter gut motility and secretion, leading to symptoms such as abdominal pain and bloating. Moreover, stress can also affect the gut microbiota, the community of microorganisms living in our gut. An imbalance in the gut microbiota, known as dysbiosis, has been linked to both IBS and anxiety.
On the other hand, IBS can also contribute to the development of anxiety. The chronic nature of IBS and the discomfort associated with its symptoms can lead to increased stress and anxiety levels. Furthermore, the gut microbiota can influence brain function and behavior through the production of various substances, including neurotransmitters and metabolites. Dysbiosis can therefore affect mood and anxiety levels, further highlighting the intricate relationship between the gut and the brain.
The understanding of the mind-gut axis has opened up new avenues for the treatment of IBS and anxiety. For instance, interventions aimed at reducing stress and anxiety, such as cognitive-behavioral therapy and mindfulness-based therapies, have been shown to improve IBS symptoms. Similarly, interventions targeting the gut microbiota, such as probiotics and dietary modifications, can also have beneficial effects on both IBS and anxiety.
In conclusion, the mind-gut axis plays a pivotal role in the complex relationship between IBS and anxiety. The bidirectional communication between the brain and the gut can influence both gut health and mental health, highlighting the importance of a holistic approach to health and wellbeing. While more research is needed to fully understand this complex relationship, the current evidence underscores the potential of targeting the mind-gut axis in the management of conditions like IBS and anxiety.